This page contains a brief description of terms I often use, it exists to assist my clients who are interested in doing some research. If you have questions please contact me. You can find more pages like this by click on the research and resources category or by scrolling down to the tags then finding a specific terms, such as “vagus”, click on that to read other articles relating to that topic.
The autonomic nervous system (ANS) is the part of the nervous system (NS) that supplies the internal organs, including the blood vessels, stomach, intestine, liver, kidneys, bladder, genitals, lungs, pupils, heart, and sweat, salivary, and digestive glands.
The autonomic nervous system has two main divisions: Sympathetic nervous system (SNS) and Parasympathetic nervous system (PNS).
The sympathetic nervous system (SNS) activates what is often termed the fight or flight response. It prepares the body for stressful or emergency situations, it increases heart rate and the force of heart contractions, and widens (dilates) the airways to make breathing easier. It causes the body to release stored energy. Muscular strength is increased. The SNS also causes palms to sweat, pupils to dilate, and hair to stand on end. It slows body processes that are less important in emergencies, such as digestion and urination. It is intended to be temporary, when an individual SNS is chronically or is often activated the body has less of a chance at achieving rest & digest (i.e. less able to detox and repair).
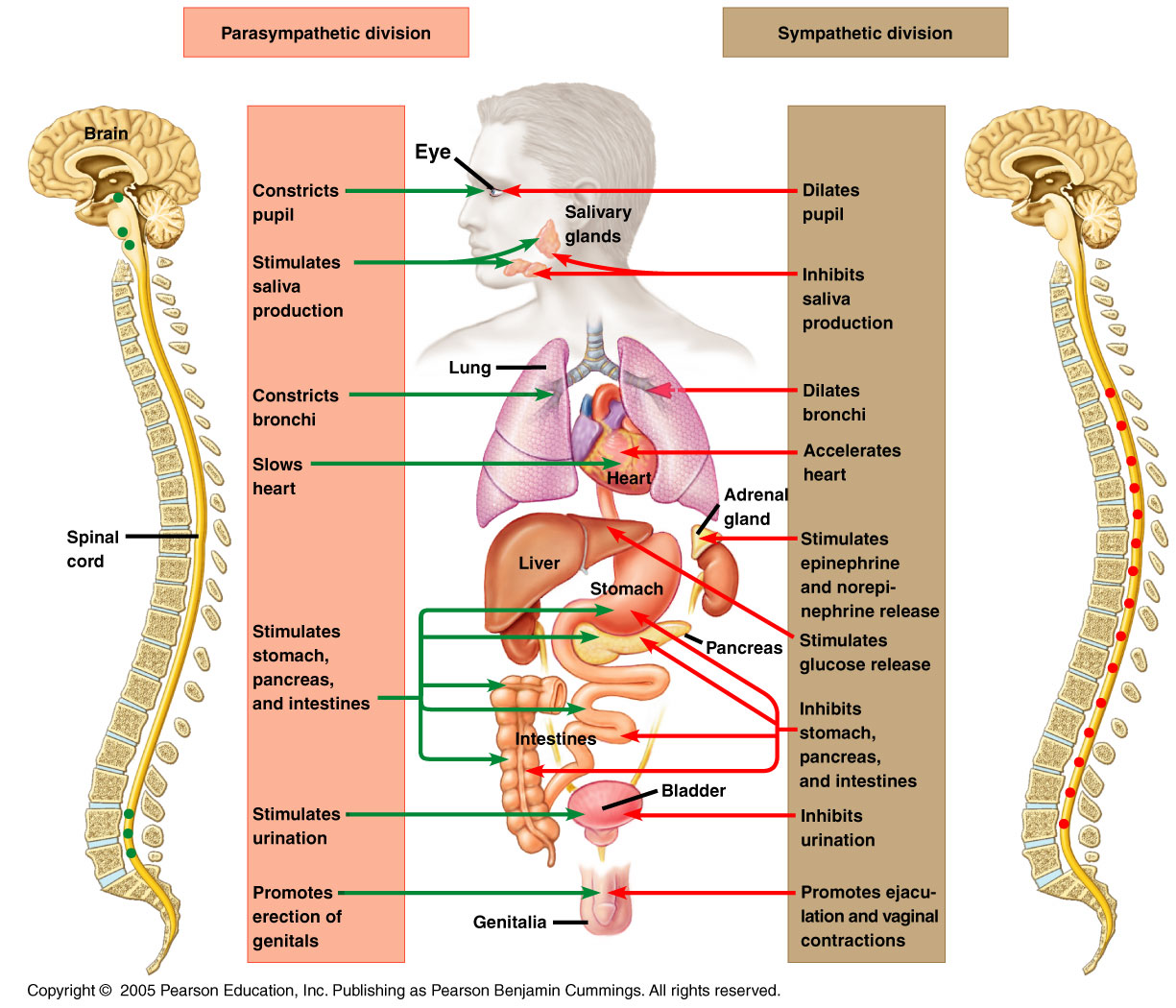
The parasympathetic nervous system (PNS) is called the rest and digest system, the parasympathetic system conserves energy as it slows the heart rate, increases intestinal and gland activity, and relaxes sphincter muscles in the gastrointestinal tract. It controls body process during ordinary situations. Generally, the parasympathetic division conserves energy and restores the body. It slows the heart rate and decreases blood pressure. It stimulates the digestive tract to process food and eliminate wastes. Energy from the processed food is used to restore and build tissues.
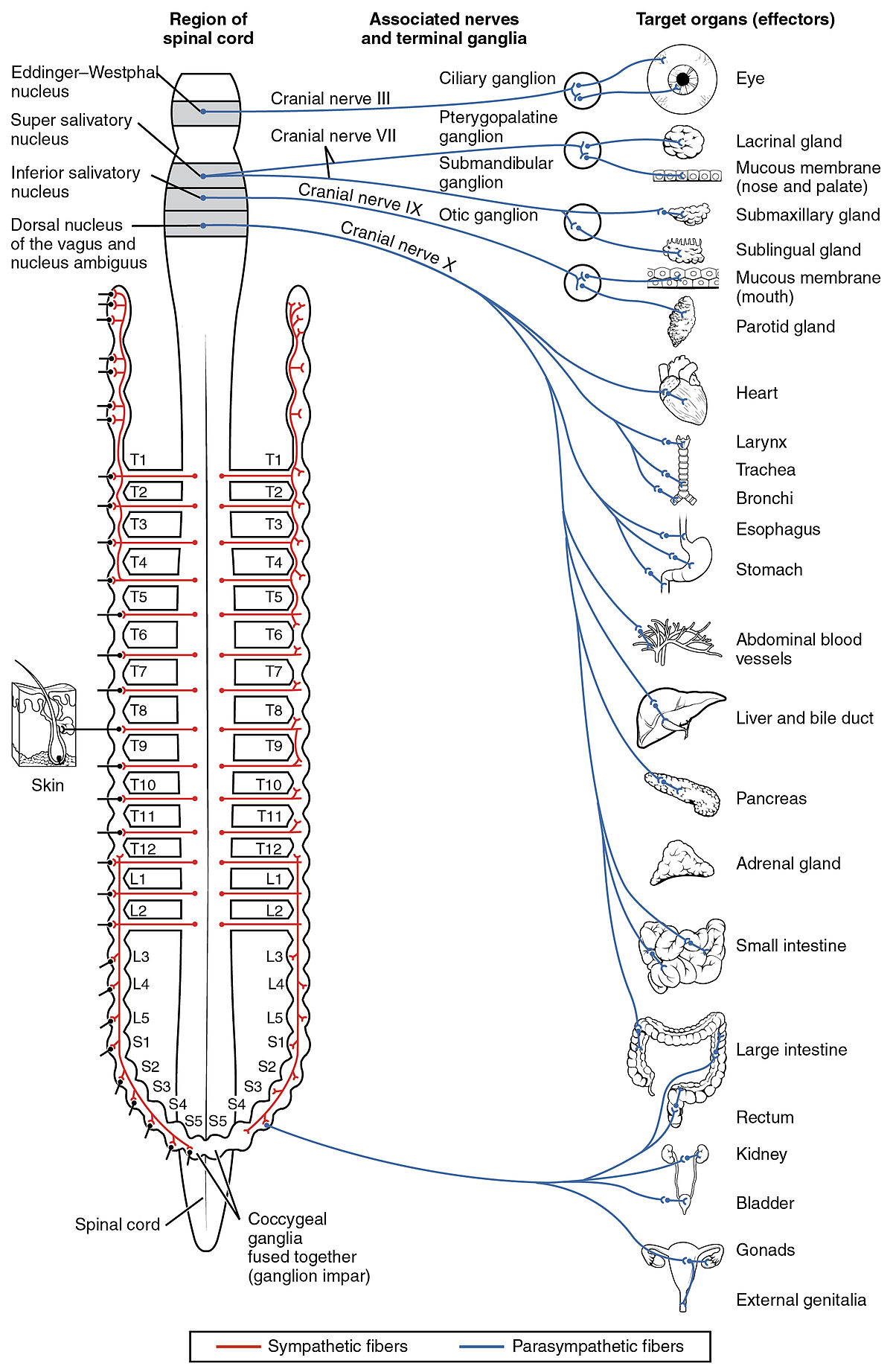
The vagus nerve: Preganglionic parasympathetic fibres of the 10th cranial or CN X (vagus) nerve arise from two different sites in the medulla oblongata. It interfaces with parasympathetic control of the heart, lungs, and digestive tract. The vagus nerves are paired; however, they are normally referred to in the singular. It is the longest nerve of the autonomic nervous system in the human body. The vagus nerve also has a sympathetic function via the peripheral chemoreceptors.
Etymology: The medieval Latin word vagus means literally “wandering” (the words vagrant, vagabond, and vague come from the same root). Sometimes the right and left branches together are spoken of in the plural and are thus called vagi (/ˈveɪdʒaɪ/ VAY-jy). The vagus was also historically called the pneumogastric nerve since it innervates both the lungs and the stomach.
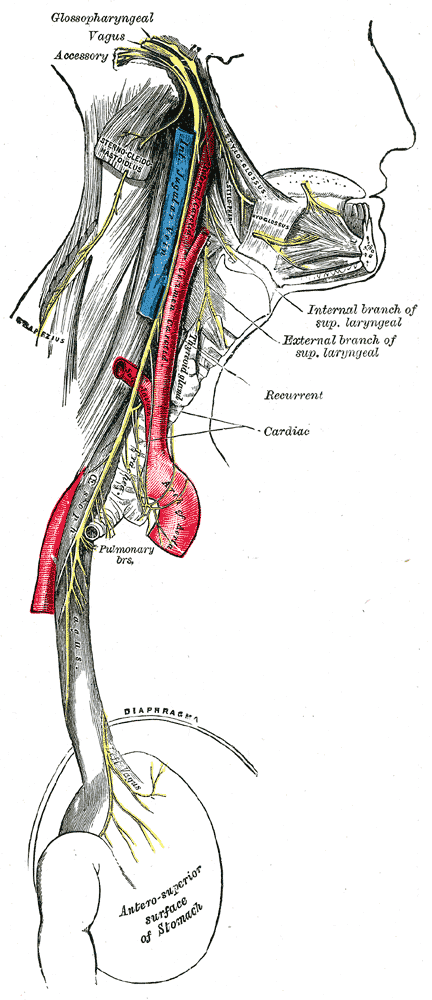
Course and distribution of the glossopharyngeal, vagus, and accessory nerves.
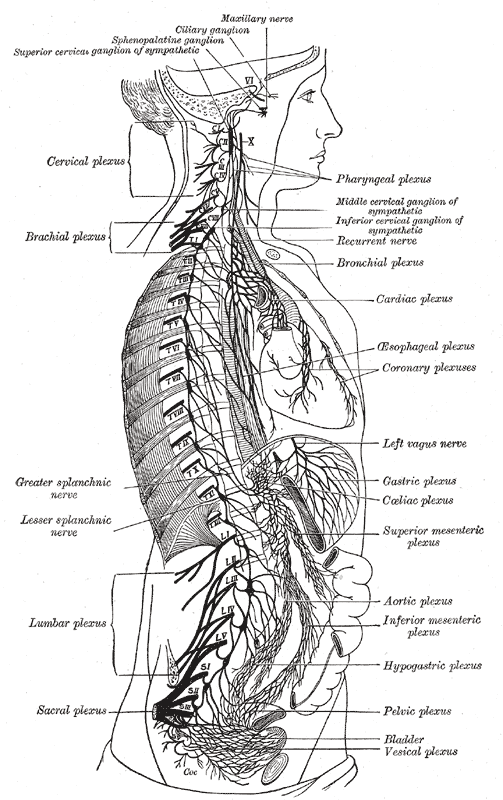
The right sympathetic chain and its connections with the thoracic, abdominal, and pelvic plexuses
The vagus nerve supplies motor parasympathetic fibers to all the organs (except the adrenal glands), from the neck down to the second segment of the transverse colon. The vagus also controls a few skeletal muscles, including:
Cricothyroid muscle
Levator veli palatini muscle
Salpingopharyngeus muscle
Palatoglossus muscle
Palatopharyngeus muscle
Superior, middle and inferior pharyngeal constrictors
Muscles of the larynx (speech).
This means that the vagus nerve is responsible for such varied tasks as heart rate, gastrointestinal peristalsis, sweating, and quite a few muscle movements in the mouth, including speech (via the recurrent laryngeal nerve). It also has some afferent fibers that innervate the inner (canal) portion of the outer ear (via the auricular branch, also known as Alderman’s nerve) and part of the meninges.
Efferent vagus nerve fibers innervating the pharynx and back of the throat are responsible for the gag reflex. In addition, 5-HT3 receptor-mediated afferent vagus stimulation in the gut due to gastroenteritis is a cause of vomiting. Stimulation of the vagus nerve in the cervix uteri (as in some medical procedures) can lead to a vasovagal response.
The vagus nerve also plays a role in satiation following food consumption.[5] Knocking out vagal nerve receptors has been shown to cause hyperphagia (greatly increased food intake).
Sympathetic function
The vagus nerve also has a sympathetic function via the peripheral chemoreceptors.[citation needed] Peripheral chemoreceptors are activated primarily due to hypoxemia. When stimulated, these chemoreceptors relay impulses throughout the vagus nerves in order to enable a vasoconstrictor response and increase blood pressure. The vagus nerve is the longest nerve in the human body.
The vagus nerve and the heart
Parasympathetic innervation of the heart is partially controlled by the vagus nerve and is shared by the thoracic ganglia. Vagal and spinal ganglionic nerves mediate the lowering of the heart rate. The right vagus branch innervates the sinoatrial node. In healthy people, parasympathetic tone from these sources are well-matched to sympathetic tone.
Physical and emotional effects
Excessive activation of the vagal nerve during emotional stress, which is a parasympathetic overcompensation of a strong sympathetic nervous system response associated with stress, can also cause vasovagal syncope due to a sudden drop in cardiac output, causing cerebral hypoperfusion. Vasovagal syncope affects young children and women more than other groups. It can also lead to temporary loss of bladder control under moments of extreme fear.
Research has shown that women having had complete spinal cord injury can experience orgasms through the vagus nerve, which can go from the uterus, cervix, and, it is presumed, the vagina to the brain.
Insulin signaling activates the adenosine triphosphate (ATP)-sensitive potassium (KATP) channels in the arcuate nucleus, decreases AgRP release, and through the vagus nerve, leads to decreased glucose production by the liver by decreasing gluconeogenic enzymes: Phosphoenolpyruvate carboxykinase, Glucose 6-phosphatase.
Clinical significance
Vagus nerve stimulation
Vagus nerve stimulation (VNS) therapy using a neurostimulator implanted in the chest is a treatment used since 1997 to control seizures in epilepsy patients and has been approved for treating drug-resistant cases of clinical depression.
VNS may also be achieved by one of the vagal maneuvers: holding the breath for a few seconds, dipping the face in cold water, coughing, or tensing the stomach muscles as if to bear down to have a bowel movement. Patients with supraventricular tachycardia,[14] atrial fibrillation, and other illnesses may be trained to perform vagal maneuvers (or find one or more on their own).
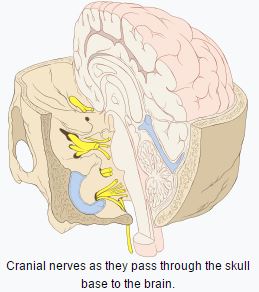
Cranial nerves
These are the nerves that emerge directly from the brain (including the brainstem), in contrast to spinal nerves (which emerge from segments of the spinal cord). 10 of 12 of the cranial nerves originate in the brainstem. Cranial nerves relay information between the brain and parts of the body, primarily to and from regions of the head and neck.
Spinal nerves emerge sequentially from the spinal cord with the spinal nerve closest to the head (C1) emerging in the space above the first cervical vertebra.
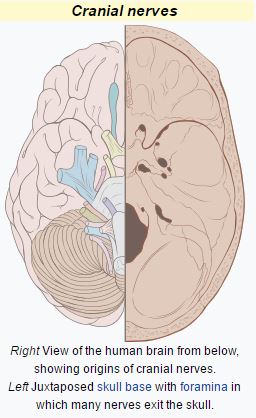
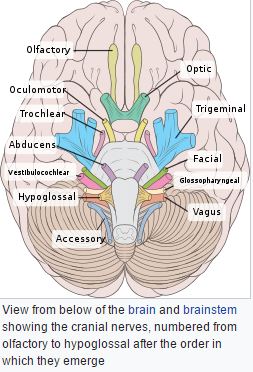
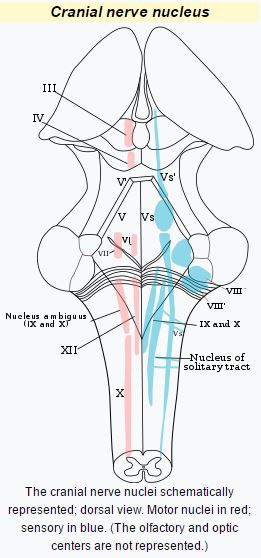
Cranial nerve nucleus
A cranial nerve nucleus is a collection of neurons (gray matter) in the brain stem that is associated with one or more cranial nerves. Axons carrying information to and from the cranial nerves form a synapse first at these nuclei. Lesions occurring at these nuclei can lead to effects resembling those seen by the severing of nerve(s) they are associated with. All the nuclei except that of the trochlear nerve (CN IV) supply nerves of the same side of the body.
Neurotransmitters
Neurotransmitters, also known as chemical messengers, are endogenous chemicals that enable neurotransmission. They transmit signals across a chemical synapse, such as a neuromuscular junction, from one neuron (nerve cell) to another “target” neuron, muscle cell, or gland cell. Neurotransmitters are released from synaptic vesicles in synapses into the synaptic cleft, where they are received by receptors on the target cells. Many neurotransmitters are synthesized from simple and plentiful precursors such as amino acids, which are readily available from the diet and only require a small number of biosynthetic steps for conversion. Neurotransmitters play a major role in shaping everyday life and functions. Their exact numbers are unknown, but more than 100 chemical messengers have been uniquely identified.
Two chemical messengers (neurotransmitters) are used to communicate within the autonomic nervous system:
Acetylcholine
Norepinephrine
Nerve fibers that secrete acetylcholine are called cholinergic fibers. Fibers that secrete norepinephrine are called adrenergic fibers. Generally, acetylcholine has parasympathetic (inhibiting) effects and norepinephrine has sympathetic (stimulating) effects. However, acetylcholine has some sympathetic effects. For example, it sometimes stimulates sweating or makes the hair stand on end.
Types
There are many different ways to classify neurotransmitters. Dividing them into amino acids, peptides, and monoamines is one approach.
Major neurotransmitters:
Amino acids: glutamate, aspartate, D-serine, γ-aminobutyric acid (GABA), glycine
Gasotransmitters: nitric oxide (NO), carbon monoxide (CO), hydrogen sulfide (H2S)
Monoamines: dopamine (DA), norepinephrine (noradrenaline; NE, NA), epinephrine (adrenaline), histamine, serotonin (SER, 5-HT)
Trace amines: phenethylamine, N-methylphenethylamine, tyramine, 3-iodothyronamine, octopamine, tryptamine, etc.
Peptides: somatostatin, substance P, cocaine and amphetamine regulated transcript, opioid peptides
Purines: adenosine triphosphate (ATP), adenosine
Others: acetylcholine (ACh), anandamide, etc.
In addition, over 50 neuroactive peptides have been found, and new ones are discovered regularly. Many of these are “co-released” along with a small-molecule transmitter. Nevertheless, in some cases a peptide is the primary transmitter at a synapse. β-endorphin is a relatively well-known example of a peptide neurotransmitter because it engages in highly specific interactions with opioid receptors in the central nervous system.
Single ions (such as synaptically released zinc) are also considered neurotransmitters by some, as well as some gaseous molecules such as nitric oxide (NO), carbon monoxide (CO), and hydrogen sulfide (H2S).
The gases are produced in the neural cytoplasm and are immediately diffused through the cell membrane into the extracellular fluid and into nearby cells to stimulate production of second messengers. Soluble gas neurotransmitters are difficult to study, as they act rapidly and are immediately broken down, existing for only a few seconds.
The most prevalent transmitter is glutamate, which is excitatory at well over 90% of the synapses in the human brain. The next most prevalent is Gamma-Aminobutyric Acid, or GABA, which is inhibitory at more than 90% of the synapses that do not use glutamate. Although other transmitters are used in fewer synapses, they may be very important functionally: the great majority of psychoactive drugs exert their effects by altering the actions of some neurotransmitter systems, often acting through transmitters other than glutamate or GABA.
Addictive drugs such as cocaine and amphetamines exert their effects primarily on the dopamine system. The addictive opiate drugs exert their effects primarily as functional analogs of opioid peptides, which, in turn, regulate dopamine levels.
Examples of important neurotransmitter actions
As explained above, the only direct action of a neurotransmitter is to activate a receptor. Therefore, the effects of a neurotransmitter system depend on the connections of the neurons that use the transmitter, and the chemical properties of the receptors that the transmitter binds to.
A few examples of important neurotransmitter actions:
Glutamate is used at the great majority of fast excitatory synapses in the brain and spinal cord. It is also used at most synapses that are “modifiable”, i.e. capable of increasing or decreasing in strength. Modifiable synapses are thought to be the main memory-storage elements in the brain. Excessive glutamate release can overstimulate the brain and lead to excitotoxicity causing cell death resulting in seizures or strokes. Excitotoxicity has been implicated in certain chronic diseases including ischemic stroke, epilepsy, amyotrophic lateral sclerosis, Alzheimer’s disease, Huntington disease, and Parkinson’s disease.
GABA is used at the great majority of fast inhibitory synapses in virtually every part of the brain. Many sedative/tranquilizing drugs act by enhancing the effects of GABA Correspondingly, glycine is the inhibitory transmitter in the spinal cord.
Acetylcholine was the first neurotransmitter discovered in the peripheral and central nervous systems. It activates skeletal muscles in the somatic nervous system and may either excite or inhibit internal organs in the autonomic system. It is distinguished as the transmitter at the neuromuscular junction connecting motor nerves to muscles. The paralytic arrow-poison curare acts by blocking transmission at these synapses.
Acetylcholine also operates in many regions of the brain, but using different types of receptors, including nicotinic and muscarinic receptors.
Dopamine has a number of important functions in the brain; this includes regulation of motor behavior, pleasures related to motivation and also emotional arousal. It plays a critical role in the reward system; Parkinson’s disease has been linked to low levels of dopamine and schizophrenia has been linked to high levels of dopamine.[20]
Serotonin is a monoamine neurotransmitter. Most is produced by and found in the intestine (approximately 90%), and the remainder in central nervous system neurons. It functions to regulate appetite, sleep, memory and learning, temperature, mood, behaviour, muscle contraction, and function of the cardiovascular system and endocrine system. It is speculated to have a role in depression, as some depressed patients are seen to have lower concentrations of metabolites of serotonin in their cerebrospinal fluid and brain tissue.
Norepinephrine which focuses on the central nervous system, based on sleep patterns, focus and alertness. It is synthesized from tyrosine.
Epinephrine which is also synthesized from tyrosine takes part in controlling the adrenal glands. It plays a role in sleep, with ones ability to become and stay alert, and the fight-or-flight response.
Histamine works with the central nervous system (CNS), specifically the hypothalamus (tuberomammillary nucleus) and CNS mast cells.
Precursor
While intake of neurotransmitter precursors does increase neurotransmitter synthesis, evidence is mixed as to whether neurotransmitter release and postsynaptic receptor firing is increased. Even with increased neurotransmitter release, it is unclear whether this will result in a long-term increase in neurotransmitter signal strength, since the nervous system can adapt to changes such as increased neurotransmitter synthesis and may therefore maintain constant firing. Some neurotransmitters may have a role in depression and there is some evidence to suggest that intake of precursors of these neurotransmitters may be useful in the treatment of mild and moderate depression.
Catecholamine and trace amine precursors
L-DOPA, a precursor of dopamine that crosses the blood–brain barrier, is used in the treatment of Parkinson’s disease. For depressed patients where low activity of the neurotransmitter norepinephrine is implicated, there is only little evidence for benefit of neurotransmitter precursor administration. L-phenylalanine and L-tyrosine are both precursors for dopamine, norepinephrine, and epinephrine.
These conversions require vitamin B6, vitamin C, and S-adenosylmethionine. A few studies suggest potential antidepressant effects of L-phenylalanine and L-tyrosine, but there is much room for further research in this area.[49]
Serotonin precursors
Administration of L-tryptophan, a precursor for serotonin, is seen to double the production of serotonin in the brain. It is significantly more effective than a placebo in the treatment of mild and moderate depression. This conversion requires vitamin C. 5-hydroxytryptophan (5-HTP), also a precursor for serotonin, is more effective than a placebo.
Neurotransmitter imbalance
Generally, there are no scientifically established “norms” for appropriate levels or “balances” of different neurotransmitters. It is in most cases pragmatically impossible to even measure levels of neurotransmitters in a brain or body at any distinct moments in time. Neurotransmitters regulate each other’s release, and weak consistent imbalances in this mutual regulation were linked to temperament in healthy people .
Strong imbalances or disruptions to neurotransmitter systems have been associated with many diseases and mental disorders. These include Parkinson’s, depression, insomnia, Attention Deficit Hyperactivity Disorder (ADHD), anxiety, memory loss, dramatic changes in weight and addictions.
Chronic physical or emotional stress can be a contributor to neurotransmitter system changes. Genetics also plays a role in neurotransmitter activities.
Apart from recreational use, medications that directly and indirectly interact one or more transmitter or its receptor are commonly prescribed for psychiatric and psychological issues. Notably, drugs interacting with serotonin and norepinephrine are prescribed to patients with problems such as depression and anxiety—though the notion that there is much solid medical evidence to support such interventions has been widely criticized.
Causes of Autonomic Nervous System Disorders
Autonomic disorders may result from disorders that damage autonomic nerves or parts of the brain that help control body processes, or they may occur on their own, without a clear cause.
Common causes of autonomic disorders are
-
Diabetes (the most common cause)
-
Peripheral nerve disorders
-
Aging
-
Parkinson disease
Other, less common causes include the following:
-
Autonomic neuropathies
-
Multiple system atrophy
-
Pure autonomic failure
-
Spinal cord disorders
-
Certain drugs
-
Disorders of the neuromuscular junction (where nerves connect with muscles), such as botulism and Lambert-Eaton syndrome
-
Certain viral infections
-
Injury to nerves in the neck, including that due to surgery
Symptoms
In men, difficulty initiating and maintaining an erection (erectile dysfunction) can be an early symptom of an autonomic disorder.
Autonomic disorders commonly cause dizziness or light-headedness due to an excessive decrease in blood pressure when a person stands (orthostatic hypotension).
People may sweat less or not at all and thus become intolerant of heat. The eyes and mouth may be dry.
After eating, a person with an autonomic disorder may feel prematurely full or even vomit because the stomach empties very slowly (called gastroparesis). Some people pass urine involuntarily (urinary incontinence), often because the bladder is overactive. Other people have difficulty emptying the bladder (urine retention) because the bladder is underactive. Constipation may occur, or control of bowel movements may be lost.
The pupils may not dilate and narrow (constrict) as light changes
The above text is a compilation of text from multiple sources posted here as an educational tool.







